Optical sensor measures blood glucose through skin
23 January 2015
Swiss research institute Empa and University Hospital Zurich have developed an optical sensor that measures blood sugar levels through the skin, without taking any blood.
It was designed to test for hypoglycemia in premature children, which can cause brain damage if left untreated for over an hour. Currently, blood samples have to be taken at regular intervals.
The Glucolight sensor’s novel measuring technology comprises: a microdialysis measuring head, developed at the University Hospital Zurich; a 'smart' membrane, developed at Empa; light sources; a pump; and a microfluidics chip with a fluorometer, also developed at University Hospital Zurich.
The membrane contains special dye molecules, known as spiropyrans. When a UV light is beamed onto these spiropyran molecules they alter their chemical structure and become charged (polar). When irradiated with visible light, they revert to their original, neutral structure. As a result, the membrane 'opens' if irradiated with UV light and glucose molecules diffuse relatively easily through the membrane from the skin. If irradiated with visible light, considerably fewer glucose molecules pass through the membrane.

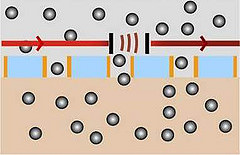
On left: Glucolight’s measuring head with the smart
membrane. On right: Diagram showing 'open' membrane letting glucose
molecule through. Credit: Empa
The measurement involves placing the measuring head, which is around three centimeters in size, on the baby’s skin and irradiating it with visible light. This allows some glucose molecules to diffuse through the membrane from the skin. On the other side of the membrane, the glucose is mixed with a fluid and pumped through the microfluidics chip, while enzymes are added to trigger a reaction.
During the reaction, fluorescence appears, which the fluorometer measures, and the computer uses the reading to calculate the glucose concentration. The process is then repeated with UV light. The computer then uses these two different readings to calculate the premature baby’s blood sugar level.
Calibration
Although skin sensors already exist, they have to be calibrated before use, which means that the skin’s permeability value needs to be known. In order to establish this, the blood sugar value has to be determined via a blood sample and the glucose concentration on the skin measured. Based on these readings, the permeability can then be calculated and the sensor calibrated.
Ongoing research
The researchers filed a patent application for Glucolight in mid-2014 and the first clinical studies are scheduled at the University Hospital Zurich for 2015. However, it could be years before the use of Glucolight becomes standard. Empa and the University Hospital Zurich are currently in negotiations with partners for the industrial production of the sensor. For the future, the researchers also envisage the use of Glucolight in other fields, such as diabetes.