Botox can slow tumour growth
22 August 2014
Research at Columbia University Medical Center and the Norwegian University of Science shows that cutting off the nerves to tumours using surgery or Botox can reduce the growth of cancer cells.
Using three different mouse models of stomach cancer, the researchers found that when they performed a procedure called a vagotomy to cut the nerves, the surgery significantly slowed tumour growth and increased survival rates.
Removing nerve connections from only one side of the stomach allowed cancer to continue growing on the other side (with the intact nerves), providing further evidence of the importance of nerves in tumour growth.
The researchers then tried to block transmission of nerve signals pharmacologically. They found that when they injected Botox into mice, the drug proved to be as effective as surgery at reducing stomach cancer growth. The research has been published in the journal Science Translational Medicine.
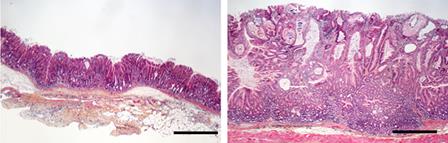
Microscope image of stomach cancer with and
without Botox injections. Cells from the anterior (left) and posterior
(right) halves of the stomach of mice with cancer. Only the anterior
stomach half was injected with Botox.
“Scientists have long observed that human and mouse cancers contain a lot of nerves in and around the tumour cells,” said Dr. Timothy C Wang, the Dorothy L. and Daniel H. Silberberg Professor of Medicine at Columbia’s Herbert Irving Comprehensive Cancer Center. “We wanted to understand more about the role of nerves in the initiation and growth of cancer, by focusing on stomach cancer.”
“We found that blocking the nerve signals makes the cancer cells more vulnerable — it removes one of the key factors that regulate their growth.”
Botox prevents nerve cells from releasing a neurotransmitter called acetylcholine. In the case of cosmetic treatment, for example, blocking acetylcholine helps to lessen facial wrinkles by causing temporary paralysis of the muscles. Because acetylcholine also ordinarily stimulates cell division, using Botox to prevent acetylcholine release might help slow the growth of cancer.
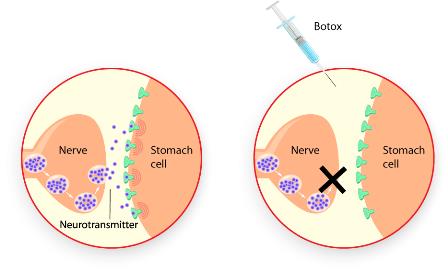
Botox is taken in by the nerves, where it
prevents the release of neurotransmitters, in this case, for a
tumour in the stomach.
Dr Wang’s team also found evidence of the effectiveness of targeting nerves for cancer treatment in human patients when they compared 37 patients who had a recurrence of stomach cancer many years after surgery. Of the 13 patients who had had a vagotomy as part of their procedure, in all but one case, tumours did not develop in regions where the nerve connections had been severed. By contrast, tumours were found in the same region of the stomach in all 24 patients who had not had a vagotomy.
Next, Dr. Wang’s team plans to investigate the effectiveness of nerve-targeted therapy used in combination with other cancer treatments. Initial experiments have shown that blocking nerves makes cancer cells more vulnerable to chemical agents. Botox® used in combination with chemotherapy in mice increases survival rates up to 35 percent, compared with chemotherapy alone.
A limitation of the current studies is that they focus primarily on early stages of stomach cancer. “In the future, we’d really like to look at how we can use this method of targeting nerves to stop the growth of more advanced tumours,” Dr. Wang said. His laboratory hopes to develop drugs that block neurotransmitter receptors. This approach would be more effective than surgery or Botox on more invasive forms on cancer, as such drugs would be able reach cells that have broken away from the main tumour.