World's first transplant of both arms
13 August 2008
The Klinikum rechts der Isar of the Technical University of Munich has successfully completed the world's first transplant of complete arms. The 15-hour operation was performed by a team of 40 people headed by PD Dr Christoph Höhnke and Prof Edgar Biemer.
Case history
The patient is a 54 year old farmer who lost both his arms at upper arm level during an accident six years ago. He had to heavily rely on help and had had two unsuccessful attempts at using artificial limbs.
He therefore approached the Clinic for Plastic Surgery and Surgery at the “Klinikum rechts der Isar” for help. He thus came into contact with a team of physicians with the ideal prerequisites for the operation: apart from a decade-long tradition in microsurgery and replantation surgery, the employees of the Clinic also have long-standing experience in interdisciplinary surgical preparation and planning — indispensable for such complex surgery.
The physicians of the Clinic for Plastic Surgery now had to initially clarify whether the future patient was physically and psychologically suitable for the difficult surgical procedure. The man was given a complete medical exam, for in order to be prepared for the suppression of the immune defence system required after transplantation, he had to be perfectly healthy. The patient also has to have a stable personality and a stable social environment.
The last phase of operative preparation was an explorative operation on the upper arm stump, during which the physicians tested to see where and how they would be able to seal off nerves and vessels during transplant. During this procedure they ascertained that the main artery in the left shoulder was occluded; this would thus require several bypasses.
Then it was solely a matter of waiting for a suitable donor, matching the host in sex, age, skin colour, size and blood group and having no injuries to the upper extremities.
The operation
The operation was started on the evening of the 25th July, around 10 pm: five teams started simultaneously in two operating theatres — one group each on the left and right side of the donor and host and an additional team removing a leg artery from the donor. First they had to expose each of the muscle ends, nerves and the vessels and prepare them for connection.
Before the donor's bones were severed, the blood vessels in the arms were filled with cooled preservation solution (perfusion). Both arms were then removed in such a way, that they accurately corresponded to the patient's arm length. Then both surgical teams connected the new body parts to the body of the host on both sides in a step-by-step procedure.
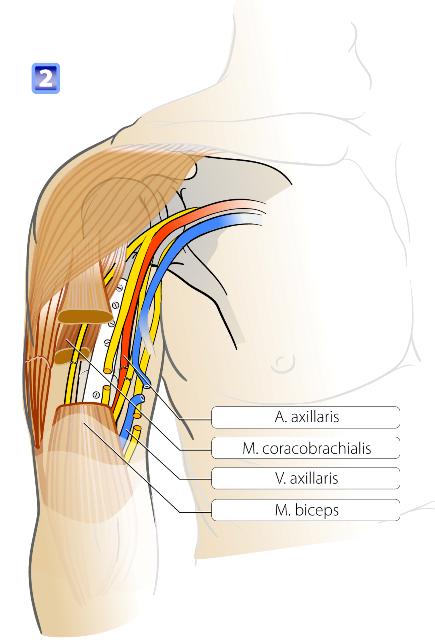
First they joined the bones together with an 8-hole plate. They then connected the arteries and veins in order to recreate circulation of the transplanted arms as quickly as possible. The left side had already been prepared with three venous bypasses.
Before completion of the anastomoses, the arms were rinsed with a special liquid to remove the preservation solution. Then the blood was released at intervals of 20 minutes; because from an anaesthetic point of view it must be ensured that the patient does not suffer acute damage from the blood flowing back from the transplants.
Figure 1. Diagram showing the arteries (red), veins (blue), nerves
(yellow) muscles and the bone plate used to join the arms.
The arms quickly took on their rosy colour and there was no significant swelling — proof for a well-functioning circulation and a short ischemia period (lack of tissue circulation).
The surgeons then sewed the muscle and tendon strands back together and finally reconnected all the nerves (nervus musculocutaneus, nervus radialis, nervus ulnaris and nervus medianus).
Next the skin could be sewn back together. Finally, a cross-joint fixateur externe was attached with pins to the lower and upper arm. This allows the arms to be suspended to avoid pressure marks. The operation was successfully concluded after 15 hours.
Current situation and further care
Not only the operation itself but also the first days afterwards continued optimally for the patient. His condition was very good under the circumstances. Now it is a matter of avoiding future wound healing disorders, infections, strong side effects caused by the drugs and, in particular, any rejective reaction (see below). Quite a number of measures were taken to this effect: close monitoring, antibiotic prophylaxis, drug monitoring and immuno-monitoring. To avoid degeneration of the muscles, these are regularly stimulated with physiotherapy, among others. The patient is also given psychological support.
Worldwide, not many hands and lower arms have been transplanted to date. The transplantation, performed in Munich, represents an even greater challenge: it also encompassed the elbow joint as well as the upper arm, signifying significantly larger regeneration areas and a more difficult immunological situation.
Allogenic upper arm transplant: an immunological challenge
In contrast to the transplant of solid organs (liver, kidney, pancreas, etc.), an extremity histologically represents heterogeneous tissue, consisting of various components with varying immunogeneity. From an immunological point of view, the focus is on
- the skin, containing cells with high immunogeneity; and
- bone marrow, which is also transferred within the scope of an upper arm transplant.
The highly immogeneous cells of the skin lead to a strong immuno-reaction in the host. During an upper arm transplant, approximately 20% of the body's entire skin surface is transplanted. At least initially, this requires a strong immunosuppressive therapy with all the possible side effects, eg infections.
Furthermore, the skin lacks a simple lab-chemical parameter (such as creatinine during a kidney transplant) to enable the recognition of an immunological reaction in the host. The diagnosis of an immunological defence reaction is thus based on the clinical assessment of the skin, regular skin biopsies and different immunological tests. This type of monitoring is far more complex than after transplantation of solid organs.
The hollow bones in the upper arm contain large volumes of bone marrow (in contrast to a hand transplant, during which hardly any bone marrow is transplanted). Bone marrow consists of immuno-competent cells, which could trigger a so-called graft-versus-host-reaction (GvHD).
This means that these cells are able to attack the host. Such an attack denotes a life-threatening situation for the host. The extent of the risk after an upper arm transplant is difficult to assess, as it has been shown that preclinical data cannot be directly transferred to the human situation. This also requires different immunological examinations in order to recognise and treat the occurrence of such a reaction at an early stage.
In principle, upper arm transplantation combines the immunological problems of bone marrow transplantation with those of solid organ transplantation. In the long run, this is joined by possible side effect caused by immuno-depressors.
From a transplantation surgeon's point of view, upper arm transplantation thus represents an interesting challenge, which also offers the opportunity of making a contribution to understanding immunological processes after transplantation.