| Diagnostic imaging, cardiology | |||
4D MRI scans of child heart help predict outcome of heart surgery29 November 2006 Atlanta, Georgia, USA. Magnetic resonance imaging (MRI) of the hearts of children with heart defects can be used to create three-dimensional models to test the effect of surgical procedures. This can help surgeons plan optimum surgery for each child’s congenital heart defect. Georgia Tech and Emory University researchers have developed an innovative new technology that will help paediatric cardiac surgeons design and test a customized surgical procedure before they ever pick up a scalpel. With a better understanding of each child’s unique heart defect, surgeons could greatly improve the likelihood that children with complex defects requiring multiple surgeries over a period of several years could have smoother recoveries and an improved quality of life after their operations.
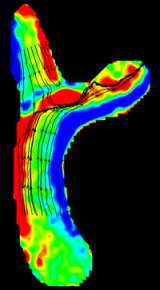
The technology, known as image-based surgical planning and developed with the help of paediatric cardiologists and paediatric surgeons at The Children’s Hospital of Philadelphia (CHOP) and Emory University, creates a three-dimensional model of the child’s heart with data from the child’s MRI scans at different times in the cardiac cycle, also called a 4D MRI. The models allow surgeons to visualize the direction of blood flow and determine any energy loss in the heart. So if a surgeon were planning a certain correction to an area of a child’s heart, a model created by the system would show the surgeon how well blood would flow through the newly configured heart. The goal of the Georgia Tech/Emory project is to create a complete system that allows surgeons to get a detailed look at the child’s heart functions with the new MRI system, design surgical procedures for optimum post-operative performance and evaluate the heart’s performance with a sophisticated blood flow computer simulation. The work was presented this month at the American Heart Association’s Scientific Sessions meeting in Chicago and has been published in Circulation and the Annals of Thoracic Surgery. “We use the MRI images and time data to create models of these children’s vascular systems and hearts to simulate how they currently work and how they could work after surgery,” said Ajit Yoganathan, Ph.D., a co-principal investigator on the project and associate chair of the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University. “The goal is to improve the quality of life for these children by understanding their current physiology and finding the best way to optimize the surgery for that particular child.” While the program isn’t yet ready for use by surgeons outside the project, it could be available in about three to five years, Yoganathan said. Although the normal heart has two ventricles or lower chambers of the heart used for pumping blood through the body, two out of every 1,000 babies in the United States are born with just one lower chamber. Considered one of the most complex congenital heart defects, a single-ventricle heart often leads to congestive heart failure if not repaired. Patients with this defect often undergo multiple surgeries to reconfigure the pulmonary and systemic systems in operations called Fontan repairs, a reconfiguration that diverts the blood flow coming to the right side of the heart directly to the lungs so that the heart no longer has to pump blood to the lungs. Staged over several years, these surgeries are a common, but not always successful, option used for treating a single-ventricle defect. After a less-than-optimal operation, children sometimes experience a reduced capacity to perform physical activities and may experience blood clotting and ventricle arrhythmias. The Georgia Tech/Emory surgery planning system could eliminate the need for additional surgeries by optimizing early surgeries. “The research is meant to get at the root of the ‘failing’ Fontan, investigating why these pumping chambers fail in the hopes of devising new strategies to give these children a second chance in life. Using advanced imaging and bioengineering tools, the project hopes to describe how blood flows in this type of circulation and how this blood flow might be altered to extend the life of the patients,” said Mark Fogel, M.D., director of cardiac MR in the Cardiac Center at Children’s Hospital and a key collaborator on the project. The Georgia Tech/Emory team began work on a system to help surgeons address the unique challenges of Fontan repair. In essence, the system determines how any geometric change in the current heart configuration will change blood flow and strength. To perfect their system, researchers combined computational and experimental studies to create a method of assessing an optimum vessel configuration. The group worked heavily with fluid dynamic studies in the lab to get the most accurate simulation of blood flow. Another tool, developed by a team led by Jaroslaw Rossignac Ph.D. in Georgia Tech’s College of Computing, is a program that allows for manipulation of a 3-D model of a patient’s cardiovascular system to try out different configurations with a mouse. Once the surgeon has the desired configuration, the new vascular configuration can then be tested with the Image-based surgical planning system to see how well the new surgical procedure would perform. Georgia Tech and Emory completed the engineering aspects of the study with assistance from the University of North Carolina at Chapel Hill. The MRI and patient studies were gathered at CHOP and Children’s Healthcare of Atlanta’s Sibley Heart Center. While the patient MRI database is currently only accessible to project participants, researchers are working with the National Institutes of Health (NIH), which funded the project, to open the database to other paediatric cardiologists and cardiac surgeons.
|