Ultrasound of inflammatory bowel disease
True to the motto ‘connecting the world of ultrasound’ the 13th Congress of the World Federation for Ultrasound in Medicine and Biology (WFUMB) will take place in Vienna on 26-29 August 2011 [1]. WFUMB 2011 is the unique joint meeting of the 23rd Congress of the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) and the 35th joint meeting of the Austrian (ÖGUM), German (DEGUM) and Swiss (SGUM) Societies for Ultrasound in Medicine. Various courses and talks will also deal with the topic contrast agents and ultrasound. One of the leading experts in the field of CEUS, Dr. Stephanie Wilson from the University of Calgary/ Canada, will be present at the WFUMB 2011 and agreed to give a short preview on her talk about inflammatory bowel disease.
19 July 2011
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and the small intestines that have a significant impact on health and quality of life. Crohn's disease (CD) and ulcerative colitis (UC) are the two most common forms of IBD.
Although the disease shows immunity alteration and dysbiosis in development, there is no known etiology or cure.
In most cases onset is in adolescence or young adult life and up to 80% of patients with CD have to face surgical bowel resection at some point due to complications such as stricture and mechanical bowel obstruction.
According to Dr. Wilson, imaging of the abdomen plays a major role in detecting IBD and in its surveillance: “Without therapy, the disease has a natural tendency for a remitting and relapsing course. As neither clinical symptoms nor inflammatory markers are reliable predictors of disease activity, there is a huge demand for imaging of the bowel to show the disease extent and activity and to monitor progression and response to therapy. Current popular therapies are aimed at mucosal healing and alteration of the natural course of the disease.”
At the moment, the gold standard in diagnosing IBD is still colonoscopy, where morphology and biopsy provide information about the patient’s condition. Ultrasound is also a very efficient way to detect IBD and is as accurate in terms of results as MR and CT.
Aside from being accurate in detecting the disease there are also other good reasons why ultrasound should be the preferred method to examine patients with known or suspect IBD.
Ultrasound works without any ionizing radiation and has no know side effects, but Dr. Wilson also points out that there are other major arguments for ultrasound as a routine method: “Excess radiation exposure from overuse of CT scans is now a well recognised outcome in this population.
Furthermore, while highly valuable, colonoscopy is invasive and
no patient will tolerate anything other than occasional repeat
examinations, emphasising the need for non-invasive and accurate
imaging techniques. Ultrasound has excellent spatial resolution
allowing for visualisation of all of the layers of the bowel wall.”
When performing ultrasound of the gastrointestinal tract there are
technical and patient-related challenges.
The technical demands include equipment requirements for a broad
range of transducer frequencies to allow for scanning of the bowel
within the focal range of the transducer so that exceptionally high
resolution can be achieved. Although all ultrasound machines have
low
frequency probes available, it is the addition of high
frequency probes, both linear and convex, which allows for good
bowel assessment, especially in thin patients.

Cross sectional and longitudinal images of the
terminal ileum show thickend bowel wall and inflammatory echogenic
fat in a patient with acute CD of the terminal ileum.
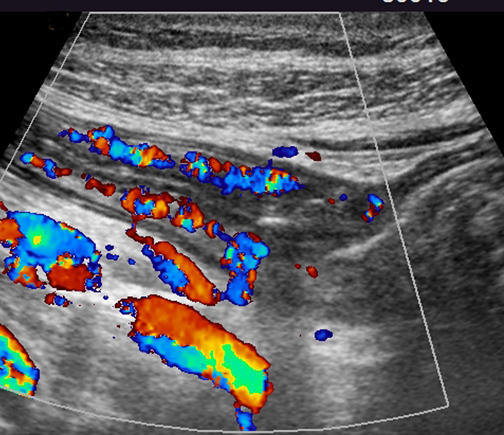
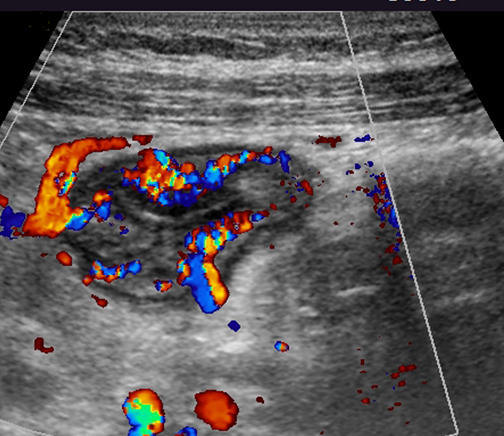
Additional Colour Doppler images show
hyperermia of the bowel
The few patient-related challenges include morbid obesity, peristalsis and gas. In general terms, excellent assessment of the gastrointestinal tract can be carried out with US in most patients.
According to Dr. Wilson, specific skills are also required on the part of the sonographer: “Reliable performance of good ultrasound examinations of the bowel requires a dedicated and skilled sonographer. Although the examinations are not so difficult, a high skill level is required to detect the subtleties of the sonographic features of disease and their complications. Sonography of the bowel is not for the faint of heart, nor for dabblers”.
The additional use of contrast agents in the detection of IBD makes a very positive contribution to the imaging technique in patients where the activity of the disease is uncertain in an identified loop of thickened bowl. This can be the case when the loop is deep in the abdomen or the signals of blood flow, shown by Doppler sonography, are too weak.
In such cases, CEUS provides the most sensitive method currently available for detecting even minor blood flow in the bowel, which as mentioned before is a relevant sign for the activity of then disease.
In terms of resolution, CEUS is a more powerful tool than common ultrasound alone for characterization of inflammatory masses: “Contrast agents are also beneficial in the resolution of an inflammatory mass as is frequently shown on imaging studies of those with IBD. While the greyscale features of abscess and phlegmon may be specific, there are many instances when this distinction cannot be made with conventional ultrasound alone. The injection of a microbubble contrast agent will show diffuse enhancement of an inflammatory phlegmonous mass, whereas an abscess will be avascular in the regions where there is pus,” said Dr. Wilson.
The last three decades have seen dramatic improvement in the
capabilities of ultrasound equipment. Current hot topics in
ultrasound include elastography, performed with direct
visualisation, as compared with other types of elastography
performed with a surface push. This
may play a potential role in
the differentiation of a fibrotic from an inflammatory stricture in
IBD.
Furthermore, the use of volumetric techniques now allows us to scan in 3D and 4D and to show volumes of data rather than a simple two dimensional display. While these current advancements are attractive and interesting, they do not as yet play much of a role in routine US of IBD.
Dr. Wilson will participate in WFUMB 2011 both as a speaker and a moderator and will mainly focus on topics such as CEUS of the liver, CEUS of the GI-tract and of course US with CEUS for assessment of complications of IBD.
More information
The 13th Congress of the World Federation for Ultrasound in Medicine and Biology (WFUMB) will take place in Vienna on 26-29 August 2011. Please see the sebsite: www.wfumb2011.org
Acknowledgements
Interview conducted by David Zizka, ESR office, and originally published in WFUMB e-newsletter 2011. Reproduced with kind permission.